Which Is A Vital Function Of The Skin
Nurses demand to understand the skin and its functions to identify and manage pare problems. This article, the first in a two-part series, looks at the skin'southward structure and key functions. This article comes with a self-assessment enabling y'all to examination your knowledge after reading it
Abstract
Skin diseases bear on 20-33% of the population at whatsoever once, and around 54% of the UK population will experience a skin condition in a given year. Nurses observe the peel of their patients daily and information technology is important they understand the skin and then they can recognise problems when they arise. This article, the first in a two-part series on the skin, looks at its structure and function.
Citation: Lawton Due south (2019) Skin i: the structure and functions of the pare. Nursing Times [online]; 115, 12, 30-33.
Author: Sandra Lawton, Queen's Nurse and nurse consultant and clinical pb dermatology, The Rotherham NHS Foundation Trust.
- This article has been double-blind peer reviewed
- Curlicue downwards to read the article or download a print-friendly PDF here (if the PDF fails to fully download please effort again using a dissimilar browser)
- Assess your cognition and proceeds CPD prove by taking the Nursing Times Cocky-assessment test
- Read function 2 of this series here
Introduction
Pare diseases affect 20-33% of the UK population at any one fourth dimension (All Parliamentary Grouping on Skin, 1997) and surveys propose around 54% of the Uk population will feel a skin condition in a given year (Schofield et al, 2009). Nurses will detect the skin daily while caring for patients and it is of import they empathise it and so they can recognise problems when they ascend.
The pare and its appendages (nails, pilus and certain glands) form the largest organ in the man body, with a surface area of 2m2 (Hughes, 2001). The skin comprises fifteen% of the total adult body weight; its thickness ranges from <0.1mm at its thinnest role (eyelids) to 1.5mm at its thickest role (palms of the hands and soles of the anxiety) (Kolarsick et al, 2011). This article reviews its structure and functions.
Structure of the skin
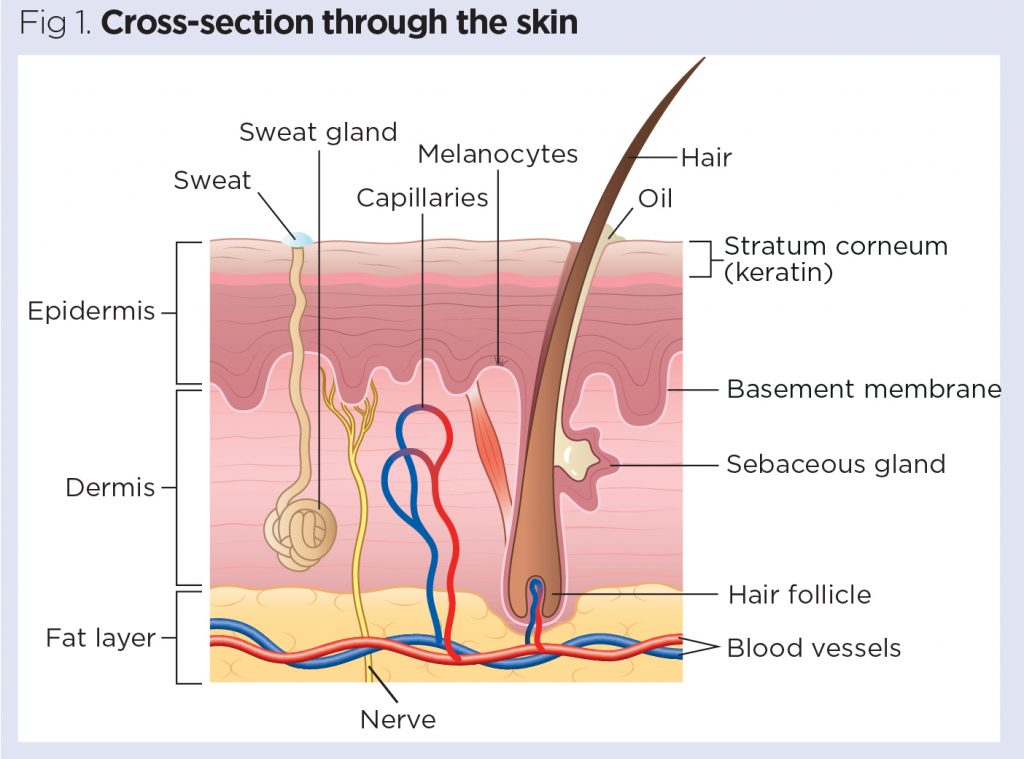
The skin is divided into several layers, as shown in Fig 1. The epidermis is composed mainly of keratinocytes. Beneath the epidermis is the basement membrane (also known as the dermo-epidermal junction); this narrow, multilayered structure anchors the epidermis to the dermis. The layer below the dermis, the hypodermis, consists largely of fat. These structures are described beneath.
Epidermis
The epidermis is the outer layer of the peel, defined equally a stratified squamous epithelium, primarily comprising keratinocytes in progressive stages of differentiation (Amirlak and Shahabi, 2017). Keratinocytes produce the protein keratin and are the major edifice blocks (cells) of the epidermis. As the epidermis is avascular (contains no blood vessels), it is entirely dependent on the underlying dermis for food delivery and waste product disposal through the basement membrane.
The prime function of the epidermis is to act as a physical and biological bulwark to the external environment, preventing penetration by irritants and allergens. At the same time, information technology prevents the loss of water and maintains internal homeostasis (Gawkrodger, 2007; Cork, 1997). The epidermis is composed of layers; most trunk parts take 4 layers, only those with the thickest skin have five. The layers are:
- Stratum corneum (horny layer);
- Stratum lucidum (but found in thick skin – that is, the palms of the hands, the soles of the feet and the digits);
- Stratum granulosum (granular layer);
- Stratum spinosum (prickle cell layer);
- Stratum basale (germinative layer).

The epidermis also contains other cell structures. Keratinocytes make upwardly around 95% of the epidermal cell population – the others beingness melanocytes, Langerhans cells and Merkel cells (White and Butcher, 2005).
Keratinocytes. Keratinocytes are formed by division in the stratum basale. As they move up through the stratum spinosum and stratum granulosum, they differentiate to course a rigid internal structure of keratin, microfilaments and microtubules (keratinisation). The outer layer of the epidermis, the stratum corneum, is composed of layers of flattened dead cells (corneocytes) that take lost their nucleus. These cells are then shed from the skin (desquamation); this consummate process takes approximately 28 days (Fig three).

Between these corneocytes in that location is a complex mixture of lipids and proteins (Cork, 1997); these intercellular lipids are cleaved down by enzymes from keratinocytes to produce a lipid mixture of ceramides (phospholipids), fatty acids and cholesterol. These molecules are bundled in a highly organised fashion, fusing with each other and the corneocytes to grade the peel'due south lipid barrier against h2o loss and penetration by allergens and irritants (Holden et al, 2002).
The stratum corneum can be visualised every bit a brick wall, with the corneocytes forming the bricks and lamellar lipids forming the mortar. Equally corneocytes contain a water-retaining substance – a natural moisturising factor – they attract and concord water. The high water content of the corneocytes causes them to not bad, keeping the stratum corneum pliable and elastic, and preventing the formation of fissures and cracks (Holden et al, 2002; Cork, 1997). This is an important consideration when applying topical medications to the peel. These are absorbed through the epidermal barrier into the underlying tissues and structures (percutaneous absorption) and transferred to the systemic circulation.
The stratum corneum regulates the amount and charge per unit of percutaneous absorption (Rudy and Parham-Vetter, 2003). One of the nigh important factors affecting this is skin hydration and environmental humidity. In healthy pare with normal hydration, medication tin can only penetrate the stratum corneum by passing through the tight, relatively dry, lipid bulwark between cells. When pare hydration is increased or the normal skin barrier is impaired every bit a upshot of pare affliction, excoriations, erosions, fissuring or prematurity, percutaneous absorption will be increased (Rudy and Parham-Vetter, 2003).
Melanocytes. Melanocytes are plant in the stratum basale and are scattered among the keratinocytes along the basement membrane at a ratio of i melanocyte to 10 basal cells. They produce the pigment melanin, manufactured from tyrosine, which is an amino acrid, packaged into cellular vesicles chosen melanosomes, and transported and delivered into the cytoplasm of the keratinocytes (Graham-Brown and Bourke, 2006). The chief office of melanin is to absorb ultraviolet (UV) radiation to protect us from its harmful furnishings.
Skin colour is determined non by the number of melanocytes, just by the number and size of the melanosomes (Gawkrodger, 2007). It is influenced by several pigments, including melanin, carotene and haemoglobin. Melanin is transferred into the keratinocytes via a melanosome; the colour of the peel therefore depends of the amount of melanin produced past melanocytes in the stratum basale and taken upwards by keratinocytes.
Melanin occurs in 2 principal forms:
- Eumelanin – exists as blackness and brown;
- Pheomelanin – provides a red colour.
Peel colour is also influenced by exposure to UV radiation, genetic factors and hormonal influences (Biga et al, 2019).
Langerhans cells. These are antigen (micro-organisms and foreign proteins)-presenting cells found in the stratum spinosum. They are part of the trunk's immune system and are constantly on the lookout for antigens in their environs so they can trap them and nowadays them to T-helper lymphocytes, thereby activating an allowed response (Graham-Chocolate-brown and Bourke, 2006; White and Butcher, 2005).
Merkel cells. These cells are only present in very small numbers in the stratum basale. They are closely associated with concluding filaments of cutaneous nerves and seem to take a role in sensation, peculiarly in areas of the body such as palms, soles and genitalia (Gawkrodger, 2007; White and Butcher, 2005).
Basement membrane zone
(dermo-epidermal junction)
This is a narrow, undulating, multi-layered structure lying between the epidermis and dermis, which supplies cohesion between the two layers (Amirlak and Shahabi, 2017; Graham-Chocolate-brown and Bourke, 2006). It is composed of 2 layers:
- Lamina lucida;
- Lamina densa.
The lamina lucida is the thinner layer and lies straight beneath the stratum basale. The thicker lamina densa is in direct contact with the underlying dermis. It undulates between the dermis and epidermis and is connected via rete ridges chosen dermal papillas, which contain capillary loops supplying the epidermis with nutrients and oxygen.
This highly irregular junction greatly increases the surface area over which the exchange of oxygen, nutrients and waste material products occurs between the dermis and the epidermis (Amirlak and Shahabi, 2017).
Dermis
The dermis forms the inner layer of the peel and is much thicker than the epidermis (ane-5mm) (White and Butcher, 2005). Situated betwixt the basement membrane zone and the subcutaneous layer, the primary part of the dermis is to sustain and support the epidermis. The main functions of the dermis are:
- Protection;
- Cushioning the deeper structures from mechanical injury;
- Providing nourishment to the epidermis;
- Playing an important part in wound healing.
The network of interlacing connective tissue, which is its major component, is fabricated up of collagen, in the primary, with some elastin. Scattered within the dermis are several specialised cells (mast cells and fibroblasts) and structures (claret vessels, lymphatics, sweat glands and nerves).
The epidermal appendages too lie inside the dermis or subcutaneous layers, but connect with the surface of the skin (Graham-Brown and Bourke, 2006).
Layers of dermis. The dermis is fabricated upward of ii layers:
- The more superficial papillary dermis;
- The deeper reticular dermis.
The papillary dermis is the thinner layer, consisting of loose connective tissue containing capillaries, elastic fibres and some collagen. The reticular dermis consists of a thicker layer of dense connective tissue containing larger blood vessels, closely interlaced elastic fibres and thicker bundles of collagen (White and Butcher, 2005). Information technology too contains fibroblasts, mast cells, nervus endings, lymphatics and epidermal appendages. Surrounding these structures is a viscid gel that:
- Allows nutrients, hormones and waste products to pass through the dermis;
- Provides lubrication between the collagen and elastic fibre networks;
- Gives bulk, assuasive the dermis to act as a shock cushion (Hunter et al, 2003).
Specialised dermal cells and structures. The fibroblast is the major jail cell blazon of the dermis and its main part is to synthesise collagen, elastin and the gluey gel within the dermis. Collagen – which gives the skin its toughness and strength – makes up 70% of the dermis and is continually cleaved down and replaced; elastin fibres give the peel its elasticity (Gawkrodger, 2007). However both are affected by increasing age and exposure to UV radiations, which results in sagging and stretching of the skin as the person gets older and/or is exposed to greater amounts of UV radiation (White and Butcher, 2005).
Mast cells incorporate granules of vasoactive chemicals (the main i being histamine). They are involved in moderating immune and inflammatory responses in the peel (Graham-Brownish and Bourke, 2006).
Blood vessels in the dermis form a circuitous network and play an important part in thermoregulation. These vessels can exist divided into two distinct networks:
- Superficial plexus – made upward of interconnecting arterioles and venules lying close to the epidermal border, and wrapping around the structures of the dermis, the superficial plexus supplies oxygen and nutrients to the cells;
- Deep plexus – found deeper at the border with the subcutaneous layer, its vessels are more substantial than those in the superficial plexus and connect vertically to the superficial plexus (White and Butcher, 2005).
The lymphatic drainage of the skin is important, the primary function existence to conserve plasma proteins and scavenge foreign cloth, antigenic substances and bacteria (Amirlak and Shahabi, 2017).
Almost i one thousand thousand nerve fibres serve the skin – sensory perception serves a critically of import protective and social/sexual function. Complimentary sensory nerve endings are found in the dermis as well every bit the epidermis (Merkel cells) and detect pain, itch and temperature. There are as well specialised receptors – Pacinian corpuscles – that detect pressure and vibration; and Meissner's corpuscles, which are touch-sensitive.
The autonomic nerves supply the blood vessels and sweat glands and arrector pili muscles (attached to the hair) (Gawkrodger, 2007).
Hypodermis
The hypodermis is the subcutaneous layer lying below the dermis; it consists largely of fat. It provides the main structural support for the skin, as well as insulating the body from cold and aiding shock absorption. It is interlaced with claret vessels and nerves.
Functions of the skin
The peel has three chief functions:
- Protection;
- Thermoregulation;
- Sensation.
Within this, information technology performs several important and vital physiological functions, as outlined below (Graham-Dark-brown and Bourke, 2006).
Protection
The peel acts as a protective barrier from:
- Mechanical, thermal and other physical injury;
- Harmful agents;
- Excessive loss of moisture and protein;
- Harmful effects of UV radiation.
Thermoregulation
Ane of the skin's of import functions is to protect the body from cold or heat, and maintain a constant core temperature. This is achieved by alterations to the blood menses through the cutaneous vascular bed. During warm periods, the vessels dilate, the skin reddens and beads of sweat form on the surface (vasodilatation = more than claret flow = greater direct estrus loss). In common cold periods, the blood vessels tuck, preventing heat from escaping (vasoconstriction = less claret flow = reduced heat loss). The secretion and evaporation of sweat from the surface of the pare too helps to absurd the body.
Sensation
Skin is the 'sense-of-affect' organ that triggers a response if we touch on or feel something, including things that may cause pain. This is important for patients with a skin condition, as pain and itching can be extreme for many and crusade nifty distress. Likewise impact is important for many patients who feel isolated by their peel as a effect of color, disease or the perceptions of others as many experience the fact that they are seen as dingy or contagious and should not be touched.
Immunological surveillance
The skin is an of import immunological organ, made up of key structures and cells. Depending on the immunological response, a variety of cells and chemical messengers (cytokines) are involved. These specialised cells and their functions volition be covered afterward.
Biochemical functions
The skin is involved in several biochemical processes. In the presence of sunlight, a form of vitamin D called cholecalciferol is synthesised from a derivative of the steroid cholesterol in the skin. The liver converts cholecalciferol to calcidiol, which is so converted to calcitriol (the active chemic form of the vitamin) in the kidneys. Vitamin D is essential for the normal absorption of calcium and phosphorous, which are required for healthy basic (Biga et al, 2019). The peel besides contains receptors for other steroid hormones (oestrogens, progestogens and glucocorticoids) and for vitamin A.
Social and sexual role
How an individual is perceived past others is important. People make judgements based on what they meet and may course their commencement impression of someone based on how that person looks. Throughout history, people have been judged considering of their peel, for case, due to its colour or the presence of a skin condition or scarring. Skin atmospheric condition are visible – in this skin-, beauty- and epitome-conscious society, the manner patients are accepted past other people is an important consideration for nurses.
Summary
This article gives an overview of the construction and functions of the skin. Part 2 will provide an overview of the accessory structures of the skin and their functions.
Primal points
- The peel is the largest organ in the homo body
- Approximately one-half of the U.k. population volition experience a skin status in any given year
- Nurses observe patients' skin daily, so need to be able to identify problems when they arise
- Key functions of the peel include protection, regulation of body temperature, and awareness
- How others respond to people who have pare conditions is an important consideration for nurses

- Test your cognition with Nursing Times Cocky-cess after reading this article. If you score fourscore% or more, y'all volition receive a personalised certificate that you can download and store in your NT Portfolio as CPD or revalidation testify.
- Accept the Nursing Times Self-assessment for this commodity
References
All Parliamentary Group on Pare (1997) An Investigation into the Adequacy of Service Provision and Treatments for Patients with Skin Diseases in the United kingdom of great britain and northern ireland.
Amirlak B, Shahabi Fifty (2017) Skin Anatomy.
Biga LM et al (2019) Beefcake and Physiology.The integumentary organization five.1: layers of the skin.
Cork MJ (1997) The importance of skin barrier function. Journal of Dermatological Handling; 8: Suppl 1, S7-S13.
Gawkrodger DJ (2007) Dermatology: An Illustrated Colour Text. Edinburgh: Churchill Livingstone.
Graham-Brownish R, Bourke J (2006) Mosby's Colour Atlas and Text of Dermatology. London: Mosby.
Holden C et al (2002) Advised best exercise for the utilise of emollients in eczema and other dry out peel atmospheric condition. Journal of Dermatological Treatment; 13: iii, 103-106.
Hughes East (2001) Pare: its structure, office and related pathology. In: Hughes E, Van Onselen J (eds) Dermatology Nursing: A Applied Guide. Edinburgh: Churchill Livingstone.
Hunter J et al (2003) Clinical Dermatology. Oxford: Blackwell Scientific discipline.
Kolarsick PAJ et al (2011) Anatomy and physiology of the skin. Journal of Dermatology Nurses' Clan; 3: 4, 203-213.
Rudy SJ, Parham-Vetter PC (2003) Percutaneous assimilation of topically practical medication. Dermatology Nursing; 15: 2, 145-152.
Schofield J et al (2009) Pare Conditions in the UK: A Health Care Needs Assessment.
White R, Butcher M (2005) The construction and functions of the skin. In: White R (ed) Pare Intendance in Wound Management: Assessment, Prevention and Treatment. Aberdeen: Wounds Britain.
Source: https://www.nursingtimes.net/clinical-archive/dermatology/skin-1-the-structure-and-functions-of-the-skin-25-11-2019/
Posted by: klattcaterneved45.blogspot.com

0 Response to "Which Is A Vital Function Of The Skin"
Post a Comment